Health risks associated with long-term use.
Written by Tracy Everhart
What are Proton Pump Inhibitors?
The first proton pump inhibitor (PPI) was introduced to the market in 1989 and since that time, they have become one of the highest grossing medications in the U.S. In 2017, they held the largest market share among all prescription medications in North America. Many of the commonly know PPIs are available by prescription and over-the-counter forms. Some of these include:
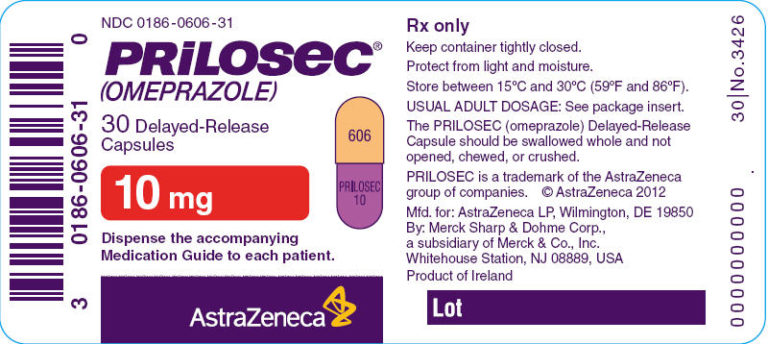
- omeprazole (Prilosec®)
- lansoprazole (Prevacid®)
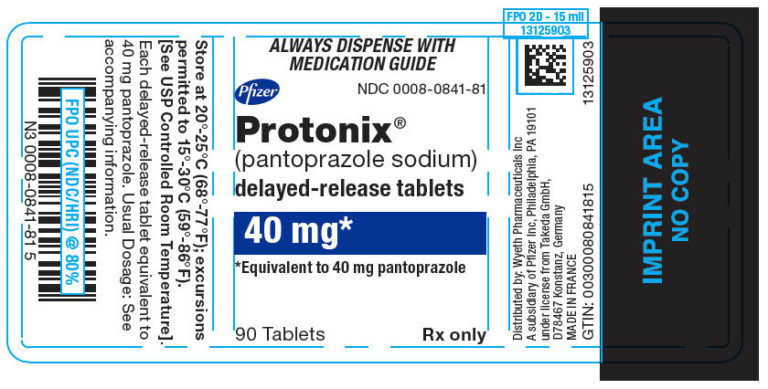
- pantoprazole (Protonix®)
- esomeprazole (Nexium®)


This class of medications are designed to manage the symptoms of gastroesophageal reflux disease (GERD), as well as other acid-related disorders (heart burn, peptic ulcers) and are the most potent inhibitors of acid secretion available. PPIs work by blocking the “proton pump” (H+/K+ ATPase) in your stomach and provide a pronounced and long-lasting reduction of stomach acids (up to 36 hours). They have also been effective in treating ulcers associated with the use of nonsteroidal anti-inflammatory drugs (NSAIDs) and for prophylactic treatment with patients that are taking NSAIDs and low-dose aspirin.
Common Side Effects of PPIs
PPIs are generally well-tolerated when taken as prescribed and for their intended use. However, like any other drug, they do pose the risk of side effects. The common side effects from short-term use of PPIs include:
- Headache
- Abdominal pain
- Nausea
- Vomiting
- Constipation
- Diarrhea
- Flatulence
- Fever
- Rash
As mentioned above, short term use of PPIs is relatively safe. Though long term use of these drugs has shown to cause numerous adverse effects, some life-threatening. They also interact with several other drugs and can reduce or inhibit that drug’s efficacy.
Severe Adverse Effects With Long-term PPI Use
The FDA has recognized the dangers associated with the long-term use of PPIs and has indicated that they are used for only four or eight weeks, depending on the condition. Despite the evidence from current research, millions of people continue to be prescribed and take these medications on a continuous basis. In some cases, these patients have been taking PPIs for years and even decades.
PPI Use Leads to Gastrointestinal
Disease and Disorders
Disease and Disorders
Chronic Hypergastrinemia
When PPIs are discontinued (even after a short course of treatment) they gastric acid will rebound causing GERD symptoms to worsen. In addition, hypergastrinemia can cause cells (parietal cells) in the stomach to enlarge and stop functioning. If these cells stop functioning, they no longer produce gastric acid and prevents the breakdown of proteins in the small intestine.
The use of PPIs also causes other cells (enterochromaffin-like cells) to enlarge and undergo an increased reproduction rate. Often this is the initial stage in the development of cancer. Recent studies have shown a link between PPI use and gastric neuroendocrine tumors (NETs), gastric adenocarcinomas and Barrett’s esophagus progression gastric cancers as a result of hypergastrinemia.
Atrophic Gastritis
Atrophic gastritis is a chronic inflammatory disease of the stomach due to infection with Helicobacter pylori. Recent studies have determined that patients receiving long-term PPI treatment are at a higher risk of developing this disease. This is due to the changes in the pH levels within the stomach that allow the growth of this particular bacteria. H. pylori infection also results in damage to gastric cells and eventually hypergastrinemia. In addition, an association between chronic hypergastrinemia and colon carcinoma was reported as early as 1998. This was based on a large prospective epidemiologic study of H. pylori-infected patients.
PPIs are Associated with a Risk of Cardiovascular Events
Myocardial Infarction
A meta-analysis included 33,492 patients in 4 randomized controlled trials and 8 controlled observational studies explained that patients receiving dual anti-platelet therapy (aspirin and clopidogrel) are typically prescribed a PPI to counteract the adverse effects of these drugs. They found that compared with placebo, PPIs increased the occurrence of major adverse cardiac events (MACE) including myocardial infarction.
Ischemic Stroke
A study published in 2018 analyzed the use of proton pump inhibitors (PPIs) and their association with an increased risk of ischemic stroke. A total of 244,679 individuals were included in the study and approximately 44 percent of these subjects were prescribed a PPI. found an association between use of PPIs and increased risk of first-time ischemic stroke. They also found a positive dose-response relationship between PPI dose and stroke risk.
PPI Use Causes an Increased Risk of Infection
Community-Acquired Pneumonia (CAP)
A meta-analysis conducted in 2011 which included eight observational studies suggested that PPI use was associated with a 27% increased risk for either hospital or community-acquired pneumonia (CAP). There were 31 studies that were reviewed, and their recommendations were that given the potential for these adverse effects, clinicians should use caution in prescribing PPI drugs for patients at risk.
Another systematic review of 33 studies and meta-analysis of 26 studies demonstrated a 1.5-fold increased risk of CAP with outpatient PPI therapy. PPI therapy was also associated with an increased risk for hospitalization with CAP (1.6-fold). The cause of this currently unknown but one theory is that PPIs decrease gastric acidity and alter the normal balance of gut flora. It is hypothesized that minute amounts of this gut flora are aspirated into the respiratory system and lead to infection.
C difficile Infections
The FDA issued a Drug Safety Communication in 2012 that warned of the increased risk of Clostridium difficile–associated diarrhea (CDAD) related to the use of both prescription and OTC PPIs. The communication encouraged patients to seek immediate medical care if they used PPIs and develop diarrhea that did not improve, for it may be the result of PPI-induced C. difficile infection.
They based this information on the results of ongoing studies. The studies that the FDA reviewed included a total of 28 observational investigations that were described in 26 separate publications. Twenty-three of the studies showed a greater risk of C. difficile infection or disease, including CDAD, associated with PPI exposure compared to no PPI exposure.
PPI Use is Linked to an Increased Risk of Fracture
In 2011, the FDA released a Drug Safety Communication warning of the increased risk of osteoporosis and fractures due to long-term use of PPIs. This communication was based on FDA’s review of several epidemiological studies that found an increased risk of fractures of the hip, wrist, and spine with the use of PPIs.
In these studies, the majority of the patients were over 50 and were prescribed PPIs. This is important, in that, prescription proton pump inhibitors are a higher dose than over-the-counter (OTC) proton pump inhibitors. These same study subjects had also been taking a PPI for at least one year. This prompted the FDA to require changes to the “Drug Fact” portion of all OTC PPIs to advise patients of the risks associated with the use of PPIs for more than 14 continuous days.
PPI Use has Been Associated with Chronic Kidney Disease
Acute Kidney Injury
In late 2014, the Food and Drug Administration (FDA) approved a label change for PPIs to include acute interstitial nephritis as a possible PPI side effect. This condition can be short or long-term and can get worse over time. It is also an important cause of acute renal failure resulting from the use of certain medications like PPIs.
A study published in 2016 in JAMA looked at the prevalence of acute kidney injury (AKI) among patients that took PPIs. These researchers observed 10,482 participants that were already enrolled in the Atherosclerosis Risk in Communities study. They found that proton pump inhibitor use was associated with a higher risk of incident chronic kidney disease (CKD).
This same study was conducted by Geisinger Health System with a replication cohort that consisted of 248,751 patients. Their findings were consistent with those of the previous study. They found that the use of PPIs was independently associated with a 20% to 50% higher risk of incident CKD. Similar findings were demonstrated for the outcome of AKI and collectively suggest that PPI use is an independent risk factor for CKD and for AKI. They feel that this may be the result of recurrent AKI.
Lawsuits Have Been Filed Against the Drug Companies That Manufacture PPIs
Numerous individual and class action lawsuits have been filed in states across the U.S. and in the federal court system.
The first class-action lawsuit filed against Astra-Zeneca (maker of Nexium® and Prilosec®) was filed in 2005. This case was related to the fact that the manufacturer released Nexium® just prior to the patent expiration of Prilosec and introduced it as a “new and improved” version of Prilosec®. Patients were encouraged to switch to this drug despite a drastic increase in price.
When it was determined that these two drugs were nearly exact, a class-action lawsuit was filed against Astra-Zeneca. The company was accused of improperly encouraging patients to switch to Nexium®, simply to increase profits. Astra-Zeneca ultimately paid $20 million to settle a class-action lawsuit. However, by then, the company was also facing medical injury lawsuits over Nexium® that were independent of the 2005 case.
In May 2010, the U.S. Food and Drug Administration (FDA) published a Safety Communication in response to research linking Nexium® to bone fractures of the hip, wrist, or spine. As a result of this communication, dozens of Nexium® bone fracture lawsuits were throughout the United States. In December 2012, these lawsuits were consolidated into a Multi-District Litigation (MDL) in the U.S. District Court for the Central District of California. This Nexium® MDL included nearly 40 individual and class action lawsuits.
In August 2017, federal cases against PPI manufacturers were consolidated into a multi-district litigation (MDL) in the U.S. District Court for the District of New Jersey (Case No. 2:17-cv-12139-CCC-MF). MDL consolidation allows for the cases to be grouped so that lawyers for both plaintiffs and defendants can concentrate their efforts and address many lawsuits at one time. At the time of the consolidation, the litigation consisted of 161 actions and the panel was informed that there would be at least 34 additional federal actions involving related issues. The latest report is that this MDL now has more than 650 lawsuits filed which are currently in the discovery stage. The defendants in these cases are AstraZeneca Pharmaceuticals LP, Procter & Gamble Co., McKesson Corp., Takeda Pharmaceuticals USA Inc., Novartis Pharmaceuticals Corp., Pfizer Inc., and Pfizer subsidiary Wyeth. The plaintiffs allege that PPIs cause kidney injuries including acute interstitial nephritis, chronic kidney disease, and end-stage renal disease.
An additional case was also added to this MDL in August 2018. The complaint alleges that a California man developed gastric cancer following long-term use of Nexium® 24HR. An association was previously suspected, particularly among individuals with Helicobacter pylori (HP) infections. However, a recent study found users of PPI drugs can face twice the risk of gastric cancer, with an even greater risk with long-term use. They also found an increased risk was there even after patients received HP infection treatment.
As of September 2018, it was estimated that there were more than 4,000 lawsuits filed in federal court against PPI manufacturers for medical injuries experienced while taking PPIs like Prilosec®, Nexium®, Prevacid®, and Protonix®. This isn’t the first time that the manufacturers of these drugs have been in court. PPI lawsuits claim that these drugs were not properly tested and that the companies that manufacture these drugs failed to adequately warn medical practitioners and the public of potential risks.
References:
http://www.gutnliver.org/journal/view.html?doi=10.5009/gnl15502
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2855237/
https://journals.sagepub.com/doi/10.1177/1756284818777943
https://www.fda.gov/Drugs/DrugSafety/ucm290510.htm#Table_3
http://www.cmaj.ca/content/183/3/310.long
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0128004
https://onlinelibrary.wiley.com/doi/abs/10.1111/aas.13094
https://www.tandfonline.com/doi/abs/10.1517/14740338.2016.1118050
https://www.researchgate.net/publication/6405875_Chronic_Hypergastrinemia_Causes_and_Consequences
https://gut.bmj.com/content/67/1/28.abstract
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5779765/
https://www.ahajournals.org/doi/abs/10.1161/circ.134.suppl_1.18462
Written by:

Tracy R Everhart, MSN, MS CAM
For more than 20 years I've had the opportunity to work in numerous rolls within the medical field, including the last 7 years as a professional medical writer. With an undergraduate degree in biology/microbiology, postgraduate education in allopathic and complementary alternative medicine, my education has afforded me career opportunities with direct patient care, medical research and clinical oversight of statewide projects to improve the health of patients of all ages. I have a broad and deep knowledge of illnesses and conditions that can affect the human body. Even more important is that I have learned traditional treatment methodologies combined with alternative forms, to make the most informed decision about options that may be available.

Get a Free PPI
Case Review
Case Review
If you are one of the thousands of people who have experienced complications after taking Prilosec®, Nexium®, Prevacid®, and Protonix®, you may be eligible to receive a compensation.


